Minor Procedure Advice
If you regularly perform office-based procedures, you will probably be familiar with most of the content below. We believe, however, that you may find some of information helpful when performing minor procedures. Please feel free to contact us to discuss specific cases as required.
Patients who are fully anticoagulated or who are on anti-platelet agents other than aspirin.
- Stop blood-thinners for an adequate amount of time prior to performing any procedure.
- Coagulation devices should be available.
Immunocompromised patients.
- It is best that immunocompromised patients have their procedures in a full sterile environment with full gowning and gloving as well as appropriate draping.
Prosthetic cardiac valves:
- A full sterile environment and appropriate peri-operative prophylactic antibiotics should be considered.
The answer to this question obviously depends on how well the procedure room is equipped and the level of training you have had in the particular procedure.
If the setting is like an operating theatre with capabilities of providing a full sterile environment with full gowning and gloving as well as appropriate draping, many procedures can be performed under local anaesthesia. These include hernia repairs, pilonidal surgery, carpal tunnel surgery, wedge excision of ingrown toenails (including nailbed down to the bone). Some of these procedures obviously require coagulation devices (monopolar / bipolar diathermy). Background training is a must and an assistant is required for most of these procedures.
In the more common setting of a small procedure room without the ability to provide a full sterile environment, only smaller procedures should be performed such as excision of skin lesions (+/- minor local flaps if you have had the training), excision of a sebaceous cyst, excision of small lipomas and drainage of small abscesses.
Drainage of a haematoma is usually not appropriate under local anaesthesia in the setting of a minor procedure room especially without coagulation devices and suction.
Removal of a foreign body that is not palpable is also not advised under local anaesthetic in a minor procedure room.
Use a fast-acting local anaesthetic such as Lignocaine (Xylocaine).
The use of adrenaline prolongs the effect of the local anaesthetic, reduces bleeding and allows you to use a larger dose of LA.
However, the use of adrenaline is contra-indicated near end-arteries such as in the digits and penis. DO NOT USE ADRENALINE AROUND END-ARTERIES.
The maximum amount of anaesthetic injected is based on the patient’s weight.
Lignocaine with adrenaline = 7mg/kg
Lignocaine without adrenaline = 3mg/kg
Bupivocaine (Marcaine) = 2mg/kg
For example:
- For a 70kg patient, using 1% Lignocaine with adrenaline
- Maximum dose in mg/kg = 7
- Maximum does in mls = 7 x (70/10) x (1/1) = 7 x 7 x 1 = 49mls
If using 2%, then the maximum dose in mls is = 7 x (70/10) x (1/2) = 24.5mls
The amount you need for most minor procedures will be much less than this. If not, then dilute the LA in saline to obtain the desired amount of infiltration required.
LA injection usually stings. This article outlines ways of possibly reducing pain associated with LA.
Only use absorbable material for placing sutures deep to the skin (eg. dermal or subcuticular or when placing a suture for control of bleeding). In operating theatre, we can use non-absorbable material for deep tissues but it is in a more controlled sterile environment and usually for deeper tissues.
The most commonly used absorbable sutures are Vicryl and Monocryl. When using Vicryl, you need 4 throws for a knot. When using Monocryl, you need 5-6 throws for a knot to avoid slipping.
Non-absorbable sutures are used for skin. Placing interrupted sutures to skin is more haemostatic than a subcuticular suture. So, if you have not used a coagulation device, it is better to use interrupted sutures to reduce the chance of post-operative bleeding.
The most common non-absorbable sutures are Nylon and Polene. Silk is not advisable as it is multi-filament and increases the risk of infection.
The number on the suture material indicates how fine the suture is. The larger, the number, the finer the suture. If a wound is under tension (which is not desirable), use a thicker suture (eg. an “0” or a “2-0”).
- The most common suture size to use for the trunk is 3-0.
- On the limbs, use 3-0 or 4-0
- On the neck, use 4-0
- On the face, use 5-0
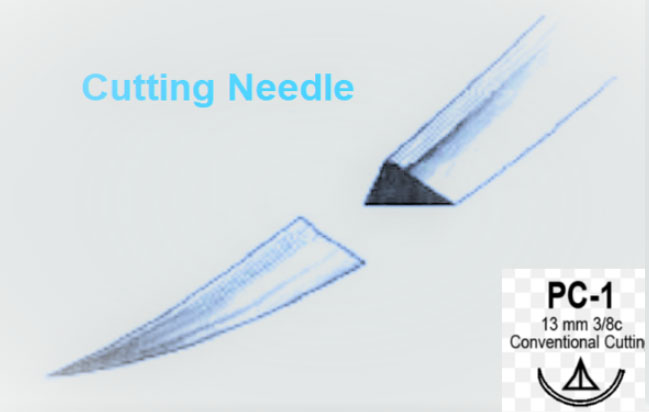
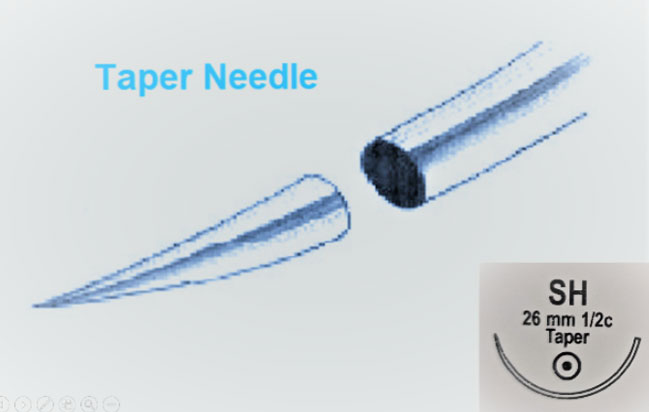
The most relevant detail about the needle in this context is what the needle looks like in cross-section. Broadly speaking, there are two main types:
1. Round body (or taper)
This is where the needle is round in cross-section. It is only sharp at the point. This means it parts the tissue as it goes through rather than cutting it. It is usually used when suturing deeper structures and when controlling bleeding. It is also useful for suturing mucosa such as the inside of the lips or for a circumcision.
Light:
Ensure adequate lighting. A headlight can be very useful (Bunnings headlights are good enough).
Bed:
Ensure the bed is at the right height and position for you.
Patient position:
Plan the patient’s position to be comfortable for both the patient and yourself.
Adequate exposure:
Ensure adequate exposure as well as protection of the patient’s clothes with the use of towels or “blueys”.
Plan your incision:
Use a permanent marker to plan your incision (it is sometimes important to re-draw after local infiltration as the markings can come off).
Local infiltration:
Clean the site with alcohol swabs. Mark the lesion. Clean around the lesion again with an alcohol swab before infiltration. Allow the local to work (see above for advice on local anaesthesia).
Get your equipment ready:
You will need:
- Trolley
- Sterile trolley cover (usually comes as part of pre-packaged dressing pack or suture pack)
- Drapes. Use the paper towel in the dressing pack for minor procedures by cutting a small window in the centre. Larger fenestrated drapes or larger sterile drapes should be used any deeper lesions particularly if deep absorbable sutures are being used.
- Preparation solution – use chlorhexidine or betadine unless the patient is allergic. Aqueous chlorhexidine (blue) is best for the face near the eyes.
- Blade – a 15 blade is best for more precise incisions and smaller lesions.
- Suture kit – Needle holder, Forceps (toothed – like a Gillies or an Adson’s), suture scissors (or dissecting scissors which can double up as suture scissors but can also be used to dissect around sub-cutaneous lesions.
- Gauze – this is very important to keep your field dry as you dissect to stay in the correct tissue plains.
- Suture material (see above for details).
- Pathology jar with formalin (preferably pre-labelled with the patient’s details).
- Dressings
If you suspect a skin lesion is a melanoma, only perform a punch biopsy. Refer to a melanoma specialist or a dermatologist.
If you are excising a non-melanoma skin cancer, make sure you have adequate margins.
Lesions on the palms, feet, lower limbs (distal to the knees) are difficult to close primarily and should be referred on to a plastic surgeon.
Local flaps are very useful but should only be done when you have had the appropriate training as they often look much easier than they are. Planning as well as knowing how much to mobilize a local flap are essential prior to embarking on these.
Most sebaceous cysts can be excised under local anaesthetic (LA).
Be careful that the LA is infiltrated around the cyst and not into the cyst. Try to infiltrate in the plain between the skin and the cyst. Most of the skin that is adherent to the cyst has to be excised to avoid leaving the capsule behind.
To avoid dog-ears at the ends of the incision, make sure the length of the wound is at least 3 times its width.
Coagulation device is usually not required but may come in handy for larger cysts or bleeding from surrounding fat if you do not stay right on the capsule during dissection.
Lubricant gel can be used like “hair-gel” to part the hair away from the cyst to minimize the area shaved.
These cysts do not usually require excision of the overlying skin unless they are large or the skin is compromised. They usually shell out like a “pearl”.
The best way to stop bleeding from the scalp is to close the wound with simple interrupted sutures (usually using 3-0 Prolene if available). Prolene is blue in colour which makes it easier to take out the sutures later on.
If a lipoma is large (≥5cm), is painful or has rapidly enlarged, investigate with an ultrasound first prior to embarking on excision. Exclude internal vascularity. These may need to be investigated further with an MRI to exclude a more sinister lesion such as a liposarcoma. DO NOT ATTEMPT TO EXCISE THESE.
Lipomas on the limbs tend to be better defined or have a nicer plain around them and are therefore easier to do under LA without necessarily needing a coagulation device. They can almost be “popped out”
Lipomas on the trunk tend to have a less defined plain around them and are more difficult to dissect They do not usually “pop-out”. Use of a coagulation device is advisable for haemostasis.
Bleeding from the skin edge will usually stop with skin closure. Use interrupted sutures rather than a sub-cuticular.
Deeper bleeding should be treated like all other surgical bleeding with:
- Direct pressure
- Ensure adequate lighting
- Ensure adequate exposure / retraction
- Use a coagulation device if available
- Place a haemostat (artery forceps) directly on the bleeder and secure with a tie or a stitch-tie.
- Place a stich-tie (or figure of eight tie) around the bleeding point using a taper needle of an absorbable suture material (eg. 3-0 Vicryl on a taper).
- DO NOT PLACE BLIND SUTURES IF EXPOSURE IS INADEQUATE OR YOU ARE UNSURE OF THE ANATOMY. You can pack a wound, place a pressure bandage and seek help if unsure.